What is Enteral Feeding?
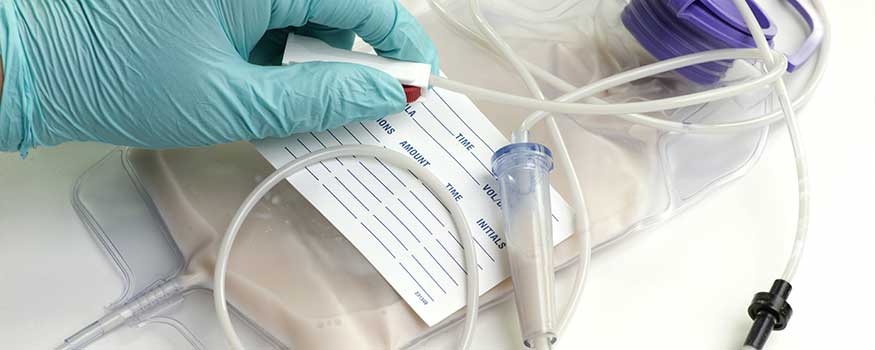
Any interventional approach to feed a patient through a feeding tube is known as enteral feeding. This kind of tube may be passed from the nose to end in the bowel or the tube can directly be placed into the stomach or the intestines by making a small incision on the skin above it.
Enteral feeding is selected when a person is unable to eat conventionally either due to any injury or pathology, however, he or she has a normal to a near-normal functioning gastrointestinal tract for digestion. This approach allows the introduction of nutrition in the individual and assists their gastrointestinal tract to continue working normally. This modality can be employed as a source of entire calorie intake or simply as a part of it in supplementary form.
Enteral feeding is always preferred over parenteral mode which is a direct introduction of nutrition to the body via an IV line unless the gastrointestinal tract is compromised. Along with delivering nutrition, enteral feeding can also be used to administer certain medications and additional fluids to the patient just like the parenteral way.
When is enteral feeding used?
There are multiple settings in which enteral feeding is required such as
- A person at risk of malnutrition: failure to thrive in young children or infants,
- Stroke patients, facing difficulty in swallowing,
- Cancer patients: inability to eat either due to nausea, vomiting or simply fatigue,
- Injury to the face or mouth,
- Patients suffering from neurological disorders,
- Patients suffering from muscular disorders,
- Bedridden patients.
However, patients with the dysfunctional digestive system are unlikely to benefit from enteral feeding. Therefore, patients with bowel obstruction, ischemic bowel, Crohn’s disease or any other serious disorder of digestive tract, etc. are not good candidates for enteral feeding.
Types of enteral feeding:
According to the American College of Gastroenterology, there are six main types of feeding tubes that can be further be classified according to the anatomical site where they end. A health care provider determines between the six of these per the time duration of the tube needed along with the current status of the digestive system and nutritional need.
The main types of enteral feeding tubes include:
- Nasogastric tube (NGT) is introduced from the nose and ends in the stomach.
- Orogastric tube (OGT) passes from mouth to the stomach.
- Nasoenteric tube starts in the nose and ends in the intestines (subtypes include nasojejunal and nasoduodenal tubes).
- Oroenteric tube connects the mouth directly to the intestines.
- The gastrostomy tube is the directly placed feeding tube in the stomach via a surgically created small hole. Subtypes include Percutaneous endoscopic gastrostomy (PEG), Percutaneous radiologic gastrostomy (PRG), and button tubes, etc.
- Jejunostomy tube: is placed through the skin of the abdomen straight into the intestines, subtypes include Percutaneous endoscopic jejunostomy (PEJ) and Percutaneous radiologic jejunostomy (PRJ) tubes.
Procedure for enteral tube placement duration of enteral feeding
- Nasal or oral tubes can be placed at the bedside or with the assistance of an endoscope. The lubricated tipped tube is inserted through the nose and is gently glided down to end in the stomach, duodenum (first part of the small intestine), or the jejunum (the second part of the intestine). A small amount of gastric or intestinal content is sucked out or an x-ray is used to confirm the site at which the tube ends. The tube is then secured with a tape at the top of the nose or mouth. Anesthesia is generally not needed for this procedure as it is simple, straightforward and only slightly uncomfortable. Feeding can be initiated immediately after the correct placement of the tube is confirmed.
- If endoscopic guidance is used, then anesthesia may or may not be used to sedate the person throughout the procedure. Here a small camera is attached to an endoscopic tube and is inserted along the feeding tube to visualize the exact placement of the tube in the stomach. At least 2-4 hours are waited out before administrating any food or fluid to provide the chance to patient to regain consciousness.
- Percutaneous or through the skin feeding tubes (Gastrostomy or jejunostomy) are inserted by making a small incision on the upper abdominal wall either by a radiologist with X-ray assistance, an Endoscopist via endoscopy or surgically by a surgeon. The patient is placed under conscious sedation or occasionally general anesthesia for this procedure. Minimum 12 hours are waited out before initiation of any type of feeding through the tube. The incision is generally very small and heals with a minimum to no scar after the tube is removed. The patient may receive oral or topical antibiotics to prevent the risk of developing any infection.
Duration of enteral feeding
- Short-term: is defined as the use of feeding tubes for less than 4 weeks.
- Long term: any duration beyond 4 weeks is considered long term enteral feeding.
The enteral feeding tube through the nose can be used for some time after which if a person is still in need of enteral feeding for longer durations, tube insertion directly through the skin to stomach is preferred.
Feed preparations
Various pre-prepared nutritionally complete feeds are easily available. These include:
- Standard enteral feeds: containing all carbohydrates, proteins, electrolytes, micronutrients, vitamins, fiber etc. that are required for a stable patient.
- Pre-digested feed: these contain pre-digested or simply essential nutrients that are easily absorbed by the gut along with variable amounts of fiber. They are selected when the improvement in absorption is the main aim of enteral feed.
Possible complications of enteral feeding:
Enteral feeding is generally regarded as a safe procedure if conducted by professional hands properly. Fortunately, no long term complications are commonly noted with enteral feeding and when normal feeding is continued after treatment only minor discomfort is observed initially in patients. However, some common complications that may arise are as follows:
- Aspiration of food into the lung and gastroesophageal reflux,
- Constipation, diarrhea, bloating or cramps,
- Improper absorption of nutrients,
- Dehydration, high blood sugar levels,
- Vitamin and mineral deficiencies and decreased liver proteins,
- Refeeding syndrome, an electrolyte imbalance that occurs if a large feed is quickly given to severely malnourished individuals,
- Wound infection at the tube insertion site in percutaneous feeding tubes,
- Nausea and vomiting if food is delivered at a fast rate,
- Tube dislodgement and leaks,
- Tube blockade, if thick consistency of food or dry meal is forced through the tube,
- Irritation in throat or nose, acute sinus infection, ulceration of larynx or esophagus, when tubes are passed via the nose.
Can enteral feeding be done at home?
Enteral feeding is a medical procedure therefore, it should always be conducted by a certified health care provider or a trained caretaker to ensure as minimum complications as possible. It can be carried out in both hospital and home settings provided adequate equipment and trained personnel are present. Many a time a home care company can be asked to provide services and equipment at home.
Feed preparation and regimens are generally advised by dieticians and prescribed by GPs. These include the formula of feeding, duration of feed, and delivery methods. It is essential to ensure the feeding content administered are adequately hydrated to prevent clogging. Feeding tubes should also be flushed with water before and after feeding, or after every 4 hours of continuous feeding.
Studies show the number of patients receiving enteral feeding at home has significantly increased in recent years. It is estimated that more than twice as many individuals receive enteral feed at home than those at hospital facilities.
Endnote:
Enteral feeding is employed mostly as a short term solution to administer nourishment when the patient is unable to do such by conventional way. Therefore, most individuals return to regular feeding once the primary complaint has been resolved with ease. In some cases, long term enteral feeding is required such as individuals with neurological or movement disorders or ones with physical disabilities and comatose patients.

References:
- Stroud M, Duncan H, Nightingale J. Guidelines for enteral feeding in adult hospital patients. Gut. 2003 Dec 1;52(suppl 7):vii1-2.
- Duro D, Collier S, Duggan C. Overview of parenteral and enteral nutrition. Up to Date online. 2006 Apr;14.
- Ojo O. The challenges of home enteral tube feeding: a global perspective. Nutrients. 2015 Apr;7(4):2524-38.
- NICE. Nutrition support in adults: oral nutrition support, enteral tube feeding, and parenteral nutrition. Clinical Guideline 32. 2006 Feb.
- Morton KH, Goodacre L. An exploration of the impact of home enteral tube feeding on the eating habits of the partners of adults receiving home enteral tube feeding. Journal of Human Nutrition and Dietetics. 2008 Aug;21(4):397-.
- Rahnemai-Azar AA, Rahnemaiazar AA, Naghshizadian R, Kurtz A, Farkas DT. Percutaneous endoscopic gastrostomy: indications, technique, complications, and management. World Journal of Gastroenterology: WJG. 2014 Jun 28;20(24):7739.