Introduction
A wound is defined as any damage or disruption to the normal anatomical structure and function of the body. It can range from a simple break in the integrity of the skin to deep damage to the structure residing underneath it. Such as tendons, muscles, vessels, nerves, internal organs and even bone. Therefore, wound healing remains a challenging clinical problem and demands efficient management to restore and protect the vital structures from further injury.
Negative pressure wound therapy(NPWT) using vacuum-assisted closure(VAC) is one of the most important modalities used in modern wound management. Multiple pieces of research show that the VAC technique for wound healing is equally or at times more effective than conventional wound closing techniques.
So today we have articulated this article to simply explain how vacuum-assisted closure facilitates wound healing and in which scenarios its use is the most beneficial.
What is wound VAC?
Vacuum-assisted closure of wound or negative pressure wound therapy is an assisted technique employed to facilitate wound healing. As the name suggests the help of a vacuum device is hired to create a negative air pressure around the wound. This proves to accelerate wound healing in many ways. For instance wound VAC:
- reduces the level of swelling,
- Keeps the wound site dry,
- Increases the blood supply towards the wound,
- Pulls the edges of the wound together to heal,
- Stimulates new tissue growth around the wound,
- And prevents infectious growth.
How is wound VAC done?
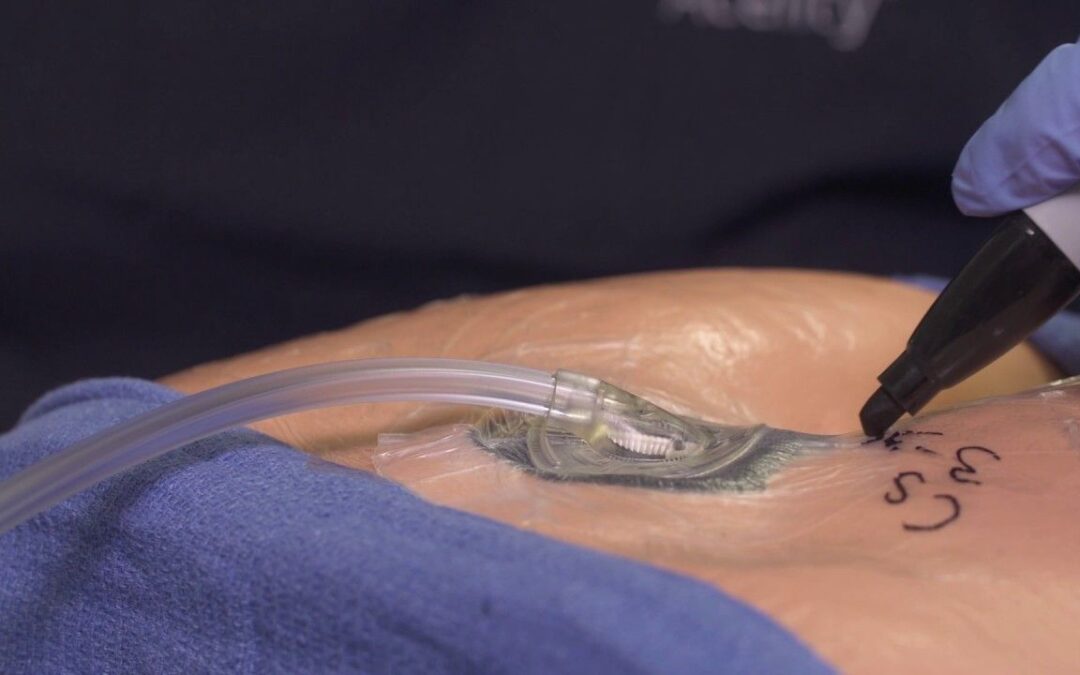
A wound VAC consists of a foam or gauze dressing applied directly to the wound, that is covered by an adhesive film to seal it. A drainage tube placed inside that is connected to a portable vacuum pump. This pump removes air pressure over the wound either cyclically or constantly. The patient is made to carry this portable pump with them at all times.
The patients might be prescribed some pain relief medications to bear any discomfort caused during the change of dressing. The dressing can be changed every 24-72 hours or two to three times a week, depending upon the nature of your wound. Wound VAC can be employed for weeks to months until the desired outcomes are achieved. The patient is also requested to reduce or stop using substances that delay the healing process such as smoking and drinking.
Indications for wound VAC?
Vacuum-assisted closure of the wound is recommended in the following conditions:
- Surgical Wounds: The incidence of surgical site infection may be as high as 40% for some surgery, and it may be even higher in individuals with preexisting medical conditions such as diabetes or cancer. A study published in 2019 reviewed multiple clinical trials to conclude that negative pressure wound therapy may decrease the incidence of surgical site infection.
- Post cesarean section; a meta-analysis found that prophylactic negative pressure therapy after cesarean is associated with reduced risk of surgical site infection and other complications.
- Pressure Injuries or Pressure Ulcers: a case report employed wound VAC technique as an alternative to the flap surgery in a nondiabetic young adult and observed healed ulcers within two months. They also estimated it to be a cheaper technique to manage pressure ulcers than flap surgeries.
- Diabetic Foot Ulcers ( DFU).
- Skin flaps and grafts.
- Burns and soft tissue trauma: A study published in 2017 validated the use of wound VAC for burn and soft tissue trauma especially in the pediatric population, stating it to be safe and effective with minimal discomfort in this age group.
Contraindications for wound VAC?
The main contraindications for use of VAC include:
- malignancy in the wound,
- wounds near joints,
- infected wounds
- fragile skin,
- wounds with poor blood supply,
- untreated osteomyelitis,
- nonenteric or unexplored fistulas,
- necrotic tissue with eschar present in the wound,
- and placement overexposed blood vessels or organs.
Disadvantages of wound VAC?
Wound VAC has some rare risks and disadvantages, these include:
- mild discomfort: a sense of stretching and pulling on the skin, but not enough to be painful.
- Bleeding: which may range from mild, moderate to severe. In such cases, more extensive management is required.
- Wound infection.
- Fistula formation: an abnormal connection formed between the skin and the intestinal tract.
- Allergy from the adhesive sheet.
- Only two case reports of sepsis and hemorrhage have been recorded, post wound VAC treatment.
- Macerated skin: softening and tearing of skin around wound due to moisture.
Can wound VAC be done at home?
It can be cried out in all settings such as a doctor’s office, hospital facility and even at home depending upon the nature and size of the wound.
The disadvantages posed by wound VAC can be reduced by carrying it out under the supervision of a trained health care provider. A trained professional can evaluate your need for a wound VAC along with following recommended protocols to ensure you do not develop any secondary complications.
This procedure can also be carried out at home once the patient is properly trained. Alongside help from a health care facility can also be employed if the patient prefers to get treated at home.

References:
- Robson MC, Steed DL, Franz MG. Wound healing: biologic features and approaches to maximize healing trajectories. Current problems in surgery. 2001;2(38):72-140.
- Alonso JE, Lee J, Burgess AR, Browner BD. The management of complex orthopedic injuries. Surgical Clinics of North America. 1996 Aug 1;76(4):879-903.
- Velnar T, Bailey T, Smrkolj V. The wound healing process: an overview of the cellular and molecular mechanisms. Journal of International Medical Research. 2009 Oct;37(5):1528-42.
- Mendez-Eastman S. Guidelines for using negative pressure wound therapy. Advances in Skin & Wound Care. 2001 Nov 1;14(6):314-23.
- Ren Y, Chang P, Sheridan RL. Negative wound pressure therapy is safe and useful in pediatric burn patients. International journal of burns and trauma. 2017;7(2):12.
- Yu L, Kronen RJ, Simon LE, Stoll CR, Colditz GA, Tuuli MG. Prophylactic negative-pressure wound therapy after cesarean is associated with reduced risk of surgical site infection: a systematic review and meta-analysis. American journal of obstetrics and gynecology. 2018 Feb 1;218(2):200-10.
- Webster J, Liu Z, Norman G, Dumville JC, Chiverton L, Scuffham P, Stankiewicz M, Chaboyer WP. Negative pressure wound therapy for surgical wounds healing by primary closure. Cochrane Database of Systematic Reviews. 2019(3).
- Batra RK, Aseeja V. Vac therapy in large infected sacral pressure ulcer grade iv—can be an alternative to flap reconstruction?. Indian Journal of Surgery. 2014 Apr 1;76(2):162-4.